Monkeypox
INTRODUCTION
"A viral zoonosis, or disease transmitted from animal to human, is monkeypox.".It exhibits symptoms similar to those of smallpox. Since smallpox was eradicated in 1980 and smallpox immunizations were subsequently stopped, monkeypox has displaced smallpox as the most important orthopoxvirus for public health. Monkeypox, which mostly affects central and west Africa, has been moving into urban areas and is frequently observed near tropical rainforests. Numerous rodent species and non-human primates serve as hosts for animals.
THE PATHOGEN
The Orthopoxvirus genus of the Poxviridae family contains the enclosed double-stranded DNA virus known as the monkeypox virus. The central African (Congo Basin) clade and the west African clade are two separate genetic clades of the monkeypox virus. The Congo Basin clade was formerly associated with more severe disease and was thought to be more contagious. The sole nation where both virus clades have been identified, Cameroon, has so far been the site of the geographic separation between the two virus clades.
NATURAL HOST OF MONKEYPOX VIRUS
It has been determined that a number of animal species are vulnerable to the monkeypox virus. There are also species such dormice, rope squirrels, tree squirrels, Gambian pouched rats, non-human primates, and others. There is still much to learn about the monkeypox virus's natural history, including its precise reservoir or reservoirs as well as the mechanisms that keep the virus circulating in the environment.
OUTBREAKS
In the Democratic Republic of the Congo, where smallpox had been eradicated in 1968, human monkeypox was found in a 9-month-old boy in 1970. Since that time, the Democratic Republic of the Congo and other rural, rain forest regions of the Congo Basin have reported the bulk of human cases, while instances are also increasingly being recorded from other parts of central and west Africa.
Monkeypox is a disease of global public health significance because it affects countries not only in West and Central Africa, but also the rest of the world. The first monkeypox outbreak outside of Africa occurred in the United States of America in 2003, and it was traced back to contact with infected pet prairie dogs. These pets were kept with Gambian pouched rats and dormice that had been imported from Ghana. This outbreak resulted in over 70 cases of monkeypox in the United States. Travelers from Nigeria to Israel in September 2018, to the United Kingdom in September 2018, December 2019, May 2021, and May 2022, to Singapore in May 2019, and to the United States of America in July and November 2021 have all been reported to have monkeypox. Multiple cases of monkeypox were discovered in several non-endemic countries in May 2022. There are currently studies being conducted to better understand the epidemiology, sources of infection, and transmission patterns.
TRANSMISSION
Animal-to-human (zoonotic) transmission can occur through direct contact with infected animals' blood, bodily fluids, or cutaneous or mucosal lesions. Evidence of monkeypox virus infection has been found in many animals in Africa, including rope squirrels, tree squirrels, Gambian pouched rats, dormice, various monkey species, and others. Monkeypox's natural reservoir has yet to be identified, though rodents are the most likely. Consuming undercooked meat and other animal products from infected animals may pose a risk. People who live in or near forested areas may be exposed to infected animals in an indirect or low-level manner.
Close contact with respiratory secretions, skin lesions of an infected person, or recently contaminated objects can result in human-to-human transmission. Droplet respiratory particle transmission typically necessitates prolonged face-to-face contact, putting health workers, household members, and other close contacts of active cases at greater risk. However, in recent years, the longest documented chain of transmission in a community has increased from 6 to 9 successive person-to-person infections. This could be due to a decline in immunity across all communities as a result of the cessation of smallpox vaccination. Transmission can also occur through the placenta from mother to foetus (resulting in congenital monkeypox) or through close contact during and after birth. While it is well known that close physical contact is a risk factor for transmission.
SIGNS AND SYMPTOMS
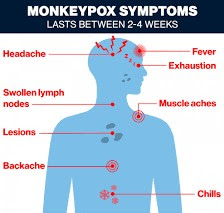
Monkeypox incubation period (time between infection and onset of symptoms) is typically 6 to 13 days, but can range from 5 to 21 days.
The infection is divided into two stages:
- The invasion period (which lasts between 0 and 5 days) is characterised by fever, severe headache, lymphadenopathy (lymph node swelling), back pain, myalgia (muscle aches), and severe asthenia (lack of energy). Lymphadenopathy distinguishes monkeypox from other diseases that may initially appear similar (chickenpox, measles, smallpox)
- The skin eruption usually begins within 1-3 days of the fever's appearance. The rash usually appears on the face and extremities rather than the trunk. It mostly affects the face, the palms of the hands, and the soles of the feet (in 75 percent of cases). Oral mucous membranes (70 percent), genitalia (30 percent), conjunctivae (20 percent), and the cornea are also affected. The rash progresses from macules (flat-based lesions) to papules (slightly raised firm lesions), vesicles (clear fluid-filled lesions), pustules (yellowish fluid-filled lesions), and crusts that dry up and fall off. The number of lesions ranges from a few hundred to thousands.
DIAGNOSIS
THERAPEUTICS
VACCINATION
Several observational studies have shown that smallpox vaccination is about 85 percent effective in preventing monkeypox. A scar on the upper arm is usually evidence of prior vaccination against smallpox. The original (first-generation) smallpox vaccines are currently unavailable to the general public. Some laboratory or health workers may have received a more recent smallpox vaccine to protect them from orthopoxviruses in the workplace. In 2019, a newer vaccine based on a modified attenuated vaccinia virus (Ankara strain) was approved for monkeypox prevention. Because of the cross-protection afforded by the immune response to orthopoxviruses, smallpox and monkeypox vaccines are developed in formulations based on the vaccinia virus.
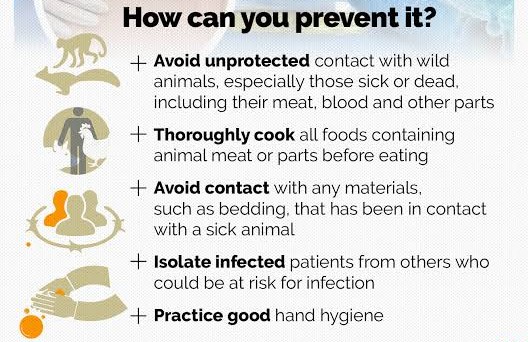
PREVENTION
The main prevention strategy for monkeypox is to raise awareness of risk factors and educate people about the steps they can take to reduce their exposure to the virus. Scientific research is currently being conducted to determine the feasibility and appropriateness of vaccination for the prevention and control of monkeypox. Some countries have policies in place or are in the process of developing policies to provide vaccine to people who may be at risk, such as laboratory personnel, rapid response teams, and health workers.
Read More Articles
Choosing the Best Pillow for Sleep Apnea
Unique Fresh Green Bean Recipes
How Long Do Lionhead Rabbits Live As Pets | Lifespan of a lionhead rabbit
Inspire Sleep Apnea Horror Stories: Triumph Over Adversity
Which Magnesium Is Best For Sleep And Anxiety | Which Is The Best Direction To Sleep
Best Time To Drink Green Tea For Weight Loss | Does Green Tea Dehydrate You
Read More Articles
Choosing the Best Pillow for Sleep Apnea
Unique Fresh Green Bean Recipes
How Long Do Lionhead Rabbits Live As Pets | Lifespan of a lionhead rabbit
Inspire Sleep Apnea Horror Stories: Triumph Over Adversity
Which Magnesium Is Best For Sleep And Anxiety | Which Is The Best Direction To Sleep
Best Time To Drink Green Tea For Weight Loss | Does Green Tea Dehydrate You


.jpeg)
.jpeg)
.jpeg)
.jpeg)